Leading Change: Resources and Information for Leaders
Busy Being Busy
This briefing invites leaders to examine how time is spent, structures and valued. The paper challenges the idea that there is not enough time suggesting instead that by using time better, and spending it more intentionally leaders can ensure there is capacity for what truly improves services and supports staff.
Competency Framework
This framework sets out the knowledge, skills and behaviours needed by professionals delivering mental health support to children, young people, and families.
The editable Competency Checklist Tool can be used by individuals and organisations to help evaluate and improve services.

Staying Safe from Suicide
80% of people in contact with mental health services who die by suicide are assessed as 'low' or 'no' risk at their last contact.
The use of static risk stratification is unacceptable. All mental health practitioners should follow this guidance instead.
Leaders Self-Assessment Tool
This tool helps you reflect on your strengths, identify challenges, and decide where to focus your time, energy, and resources.
Underspent & Overstretched:
The Missed Opportunity in Every Service Budget
Investing in people is the most sustainable way to reduce costs, retain staff, and protect services. Spend the money you have wisely and well.
Read the short (500 word) briefing to find out how.

From Increasing Awareness to Improving Outcomes:
Raising Expectations in Children's (Mental Health) Services
When it comes to the wellbeing of children, young people and families, and the accuracy and quality of the information available to those who are working with them, we must stay focused on what works.
Read the short (900 word) briefing to find out how.
A new service model for children and adolescent mental health
"A fully integrated and innovative example of a service model that operates without tiers...An inclusive, compassionate, stigma-free and youth-friendly environment...the model aims to prioritise recovery, early intervention, prevention and the development of resilience."
The Department for Education’s commitment to expanding Mental Health Support Teams (MHSTs) to reach 60% of schools is a recognition of the outcomes achieved for some young people and families through early intervention and timely access to evidence based therapies.
However, there are key challenges that must be acknowledged:
- Fragmentation of Services: In many areas, MHSTs have duplicated existing voluntary and community sector (VCSE) provision, leading to increased fragmentation. Their introduction has, at times, further confused care pathways with additional referral routes and forms, websites, phone numbers — leaving families and professionals unsure where to go or how to access the right support.
- Gaps in Provision: A significant number of children remain unsupported — considered too ‘complex’ or ‘risky’ for MHSTs, yet not meeting the threshold for NHS CYPMH (CAMHS) Services. This ‘missing middle’ continues to fall through gaps.
- Inequity in Access: With only 60% of schools set to benefit, there is a real risk of widening inequalities in access to mental health support — dependent on which schools are included, and those schools who have had MHST support since their inception for many years, whilst 40% of schools nationwide are still not expecting to be able to access support.
While the investment is welcome and not to be underestimated, it is critical that it is not used in isolation, or used in ways that increases fragmentation. To maximize this investment's potential, we must:
- Integrate Services: Ensure MHSTs complement existing provisions, avoiding duplication and demand collaboration across sectors.
- Address the 'Missing Middle': Develop pathways for children who fall between MHST and CYPMH (CAMHS) criteria, ensuring no one is left without support.
- Promote Equity: Strive for universal access, so all students, regardless of their school's inclusion in the MHST program, receive the mental health support they need.
By adopting a holistic, integrated approach, we can create a cohesive system that truly supports the mental health and well-being of all children and young people.
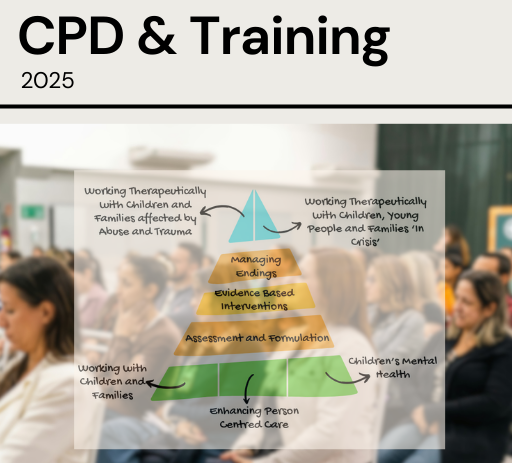
High-quality, evidence-based training is one of the most effective, and lowest-risk, investments that public services can make.
Ensuring the children and families service workforce have access to appropriate training:
• Means better outcomes for children and young people, as they are supported by staff with increased skills and confidence.
• Addresses quality or risk issues that may be linked to: gaps in skills, poor morale, burnout, sickness levels.
• Helps staff feel valued, which boosts morale and can help with staff retention.
• Strengthens the services reputation, as a place where staff are supported to access training and CPD which in turn supports recruitment.
Download the full pdf training programme to find out more below.